CMED
Cloud based Medical System for Rural Health Monitoring in Developing Countries

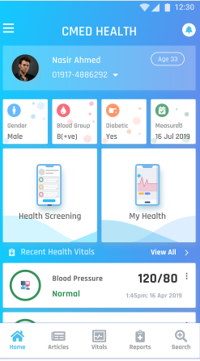
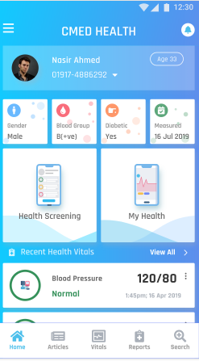
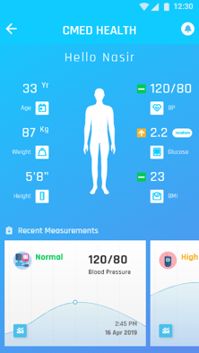
Delivering adequate healthcare in rural and remote areas of developing countries is a major challenge. CMED (Cloud-based MEDical system) addresses this by integrating cloud services with healthcare centers and portable services managed by Community Health Workers (CHWs). CMED categorizes patients into healthy, alarming, and emergency groups, ensuring timely and appropriate care. For complex cases, the system connects CHWs with specialist doctors. Using Identity-Based Encryption, CMED ensures the privacy and confidentiality of patient health information, providing a smart and secure solution to enhance healthcare accessibility for underprivileged populations.
Video
Specifications
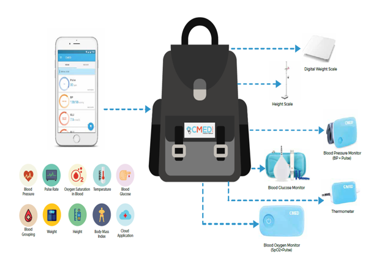
- Continuous monitoring of patients’ health status through portable and stationary healthcare systems
- Regular check-ups and real-time health data collection by Community Health Workers (CHWs)
- Evaluation of patients’ health risks based on collected data
- Categorization of patients into healthy, alarming, and emergency groups
- Provision of health education and awareness programs to patients and communities
- Promoting preventive measures and healthy lifestyle choices to reduce the risk of Non-Communicable Diseases (NCDs)
- Focused efforts on preventing NCDs like diabetes, heart disease, and stroke
- Early detection and management of risk factors through regular health assessments
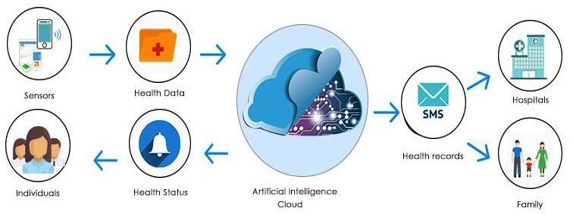
- Cloud-based system ensures that health records are accessible anytime, anywhere
- Secure storage and retrieval of patient health information
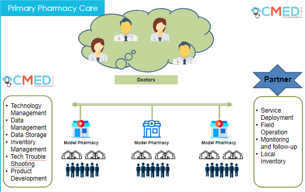
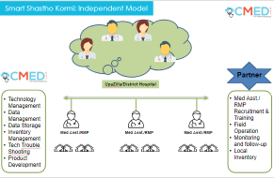
- Efficient referral system connecting CHWs with specialist doctors for complex cases
- Ensuring patients receive timely specialist care when needed
- Use of AI to predict risks of stroke, heart attack, and diabetes
- Advanced algorithms analyze health data to provide early warnings and preventive recommendations
- Comprehensive health records maintained in a secure, cloud-based system
- Ensuring healthcare providers have access to up-to-date patient information for informed decision-making
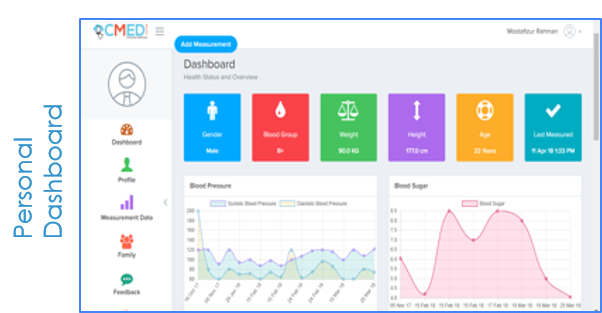
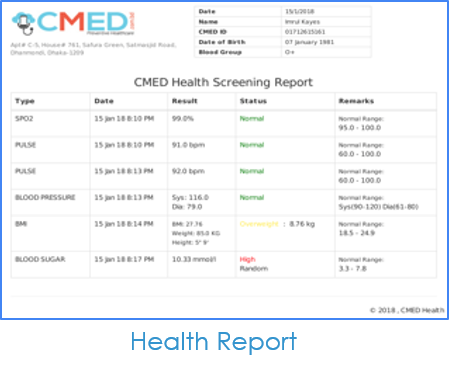
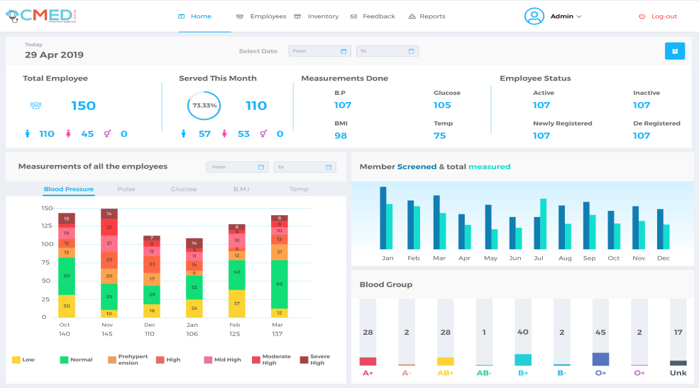
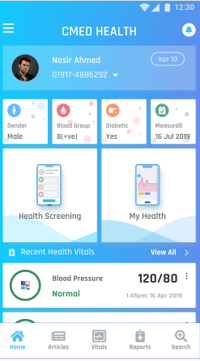
Interface
Diagrams
Publications
Kashfia Sailunaz, Musaed Alhussein, Md. Shahiduzzaman, Farzana Anowar, Khondaker Abdullah Al Mamun, CMED: Cloud based medical system framework for rural health monitoring in developing countries,Computers & Electrical Engineering, Volume 53, 2016,Pages 469-481,ISSN 0045-7906, https://doi.org/10.1016/j.compeleceng.2016.02.005. Computers & Electrical Engineering Volume 53, July 2016, Pages 469-481
Abstract
Healthcare is one of the basic human rights, but providing proper healthcare in rural remote areas of developing countries has always been a challenging task. Telemonitoring has brought some relief with limitations due to accessing patient's health information by healthcare workers and specialists, but merging it with cloud services can be an optimal solution. This proposed framework, CMED (Cloud based MEDical system), is a setup consisting of both healthcare center and a portable healthcare service with a Community Health Worker(CHW), which will sort the patients into three different categories—healthy, alarming and emergency. Upon failing to diagnose a unique problem, it will suggest and contact a specialist doctor and provide suggestions. The privacy and confidentiality of patient's health information will be secured by Identity Based Encryption. In this paper, a framework has been presented for smart and secure healthcare monitoring system for rural under privileged people in developing countries.
Digital health inclusion towards achieving universal health coverage for Bangladesh utilizing general practitioner model Moinul H. Chowdhury a, Rony Chowdhury Ripan a, A.K.M. Nazmul Islam a, Rubaiyat Alim Hridhee a, Farhana Sarker a,b, Sheikh Mohammed Shariful Islam c, Khondaker A. Mamun a,d,*
Abstract:
Bangladesh’s health care system, particularly in rural areas, experiences enormous obstacles in
providing complete preventive and primary healthcare services due to the lack of adequate healthcare facilities,
resource constraints, and a non-functional referral system. To alleviate these problems, in this study, we introduce
the digital general practitioner (GP) model for rural Bangladesh, digital platforms and present a statistical
analysis of the data that was gathered from the pilot project.
Methods: A total of 12,746 people were provided regular health services during the pilot project, from all genders
and age groups, and provided their socio-demographic and healthcare-related data. We analyzed healthcarerelated
data by carrying out both descriptive and inferential statistics.
Results: By utilizing this digital GP model, rural residents can receive routine health screenings at their homes,
identify health risks early, receive consultation and health education, and be referred to GP and upper-level
health facilities as needed. We found that hypertension was more prevalent (4.84% of the served population),
and cancer was the least prevalent of all the NCDs in the studied population (0.05% of the served population).
The population for stroke, hypertension, diabetes increased until the 50–59 age range as age increased, following
which the population proportion declined as age increased. Additionally, 3.96% of young females were severely
malnourished, comparably higher proportion than young males (2.34%).
Conclusion: NCDs such as hypertension, diabetes was prevalent among rural people. Necessary steps should be
taken to raise preventive and primary healthcare awareness among rural people.
Public interest summary: The absence of proper healthcare facilities, resource constraints, and a non-functional
referral system hamper Bangladesh’s health care system’s ability to provide comprehensive preventive and
primary healthcare services in rural area. As a result, patients develop advanced ailments, including noncommunicable
diseases (NCDs), and must seek treatment at an expensive specialty hospital. To resolve this
issue, we introduce a digital GP model for rural Bangladesh, then show digital platforms that use the concept, and
lastly summarize significant findings from the piloted digital GP model. By utilizing this digital GP model, rural
residents can receive routine health screenings at their homes, identify health risks early, receive consultation
and health education, and be referred to GP and upper-level health facilities as need. From our data analysis, we
discovered high burden of NCDs such as hypertension and diabetes in the piloted area. Necessary steps should be
taken to raise preventive and primary healthcare awareness among rural people.
Awards











Partners